Teresa Morris, Director, Advocacy & Government Relations
It is early in what has become the worst public healthcare crisis in over 100 years, As the nation continued to fight against the novel coronavirus known as COVD-19, some VA nurses received orders to deploy to hard hit areas as part of the Disaster Emergency Medical Personnel System (DEMPS) program.
Many VA healthcare workers were called to action to help in areas with large numbers of COVID-19 cases or “hot spots.” One of those hardest hit areas were Native American communities in the western United States. In May, its per capita infection rate was
one of the highest in the country
.
As part of the CARES Act (passed in March), the federal government provided $8 billion to tribal nations of which each tribe was given $600 million in relief, but for most places the money did not arrive until May.
VA was asked to step in as part of its fourth mission and healthcare workers began deploying to several Native American areas.
Many of the tribal members do not speak English and translators were often used, but VA has reported that some nurses deployed to the Native communities began learning the language and the various customs.
NOVA recognizes the exceptional work being delivered by nurses and other providers using their talent and expertise to help Native American communities during the pandemic
.

Tracey Bent
Tracey Bent, an RN from the VA Boston Healthcare System with twenty years of experience in the ED received her orders to Show Low, Arizona and immediately had to Google the location. After
a five-hour drive from Phoenix she arrived at what would be her home for two weeks in July and August. Tracey worked at Summit Healthcare Regional Medical Center, where she treated
patients from nearby Navajo and Apache Reservations. She recalled that the hospital lacked infection control measures and PPE, as well as strong COVID-19 testing and treatment. Patient testing often took 5-10 days to return results.
Staff worked 12 hour shifts with few breaks while providing additional manpower and expertise to the only hospital within hundreds of miles. Complicating things even more were the unique health challenges facing some Native American patients. “I saw patients in their 30's with pulmonary issues, liver disease, obesity and emaciation. There is a lot of poverty in the area and alcohol consumption begins at an early age,” Bent said.
At the end of her deployment, Bent believed they made a difference – “we gave the overworked nursing staff some much needed help and advocated and addressed issues with COVID-19”. When asked if she would do it again, Bent replied, “I would do it all again in a heartbeat!”

Kathy Pham
Kathy Pham, an RN from the VA Long Beach Health Care System, was deployed to Tuba City, Arizona to assist the Tuba City Regional Health Care System which is a part of Indian Health Services (IHS). VA has long worked with IHS collaborating and sharing resources to
improve the health status of American Indian and Native American Veterans. The goal is to foster an environment that brings together the strengths and expertise of each organization to actively improve the care and services provided by both.
During COVID-19, Pham assisted the local communities, nursing homes and Navajo and Hopi Natives. She found the people in the community to be humble and
modest. She commented that they value and respect their elders and do not like to ask for help. “It was an honor and a privilege to be a part of the DEMPS team that went in to help the Navajo Nation in Arizona.” Pham said.
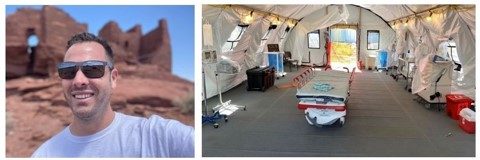
Justin Chamberland
Justin Chamberland, an RN from West Palm Beach VA Medical Center had the unique challenge of deploying to Gallup, New Mexico – which is surrounded by the largest Indian Reservation in the country. He
worked during June and July at the Gallup Indian Medical Center (GIMC) as a healthcare provider in the ED. The ED at GIMC had tents set up outside that would screen patients and treat COVID-19 patients. Chamberland was stationed at the tents for his entire deployment. While serving the Navajo Indian Nation, he asked and found out why COVID-19 was so devastating among the Navajo people. He put together information to better understand and help the unique population. Chamberland found that “most of the population live in nuclear households that includes multiple generations all living in a small area. They lack electricity and running water which makes washing their hands difficult, and many have to drive over 50 miles just to get clean water.” During his stay in New Mexico, Chamberland learned some of the language, ate blue mush and mutton and found “the Navajo were some of the most appreciative people I ever met.” Mr. Chamberland has worked at the VA for over 6 years and is currently a Clinical Nurse Coordinator for the ED.
VA continues to work in these hard-hit communities and many healthcare providers have stepped up to help. NOVA thanks these nurses for going above and beyond to take care of our nation’s Native American communities.
Photos from Native American Communities in Tuba City, AZ
