  
|
Posted By Ashley Lovelace,
Tuesday, June 16, 2020
|
If you plan to retire from the VA within the next six months, please consider joining as a NOVA Nurse Emeritus Member. https://www.vanurse.org/page/join
GOVERNANCE
The Nurse Emeritus Group is composed of NOVA members who have retired from the Department of Veterans Affairs or who are planning retirement within the next calendar year.
The Nurse Emeritus Group is an established group within the Nurses Organization of Veterans Affairs (NOVA) and, as such, adheres to all policies and practices as governed by the Bylaws of NOVA.
MISSION STATEMENT
The Nurse Emeritus Group exists to support the mission and vision of NOVA through continuing engagement of nurses who have retired or have immediate plans to retire from active employment in VA.
The Nurse Emeritus Group seeks to recognize and value the expertise of retired VA nurses through projects that support the working VA nurses and the Veterans they serve.
The Nurse Emeritus Group strives to recognize and celebrate the contribution of retired VA nurses through positive affirmation programs and projects.
What are the dues for Nurse Emeritus members? The dues for NOVA Nurse Emeritus members are $50 per year.
What does the Nurse Emeritus Group do? Nurse Emeritus projects currently include NOVA membership promotion and fundraising efforts to support nursing scholarships.
NOVA is welcoming Nurse Emeritus applications. https://www.vanurse.org/page/join
This post has not been tagged.
Permalink
| Comments (0)
|
  
|
Posted By Ashley Lovelace,
Tuesday, June 16, 2020
|
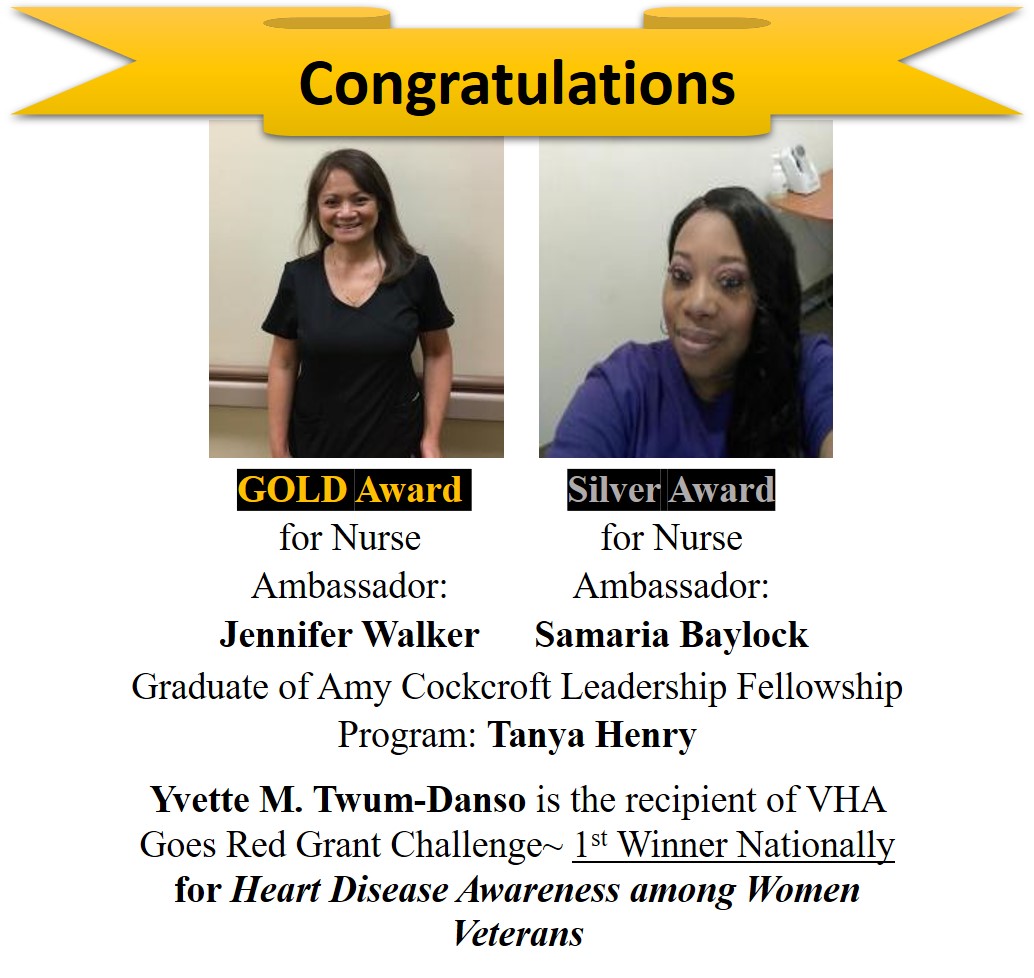
Yvette Twum-Danso, MSN, RN, CCRN, PhDc
NOVA Chapter 362
Columbia, South Carolina

Despite the COVID19 pandemic, Chapter 362 has been making the best of the situation in South Carolina. As many VA nurses celebrated nursing week in May 2020: The Year of the Nurse; the Columbia, South Carolina NOVA Nurses stayed resilient. Even though the nursing week activities were modified due to COVID19; Chapter 362 had an amazing nursing week-we celebrated with each other. We celebrated with many exciting themes: Retro White Day, NOVA Spirit Day, and Nursing Spirit Day.

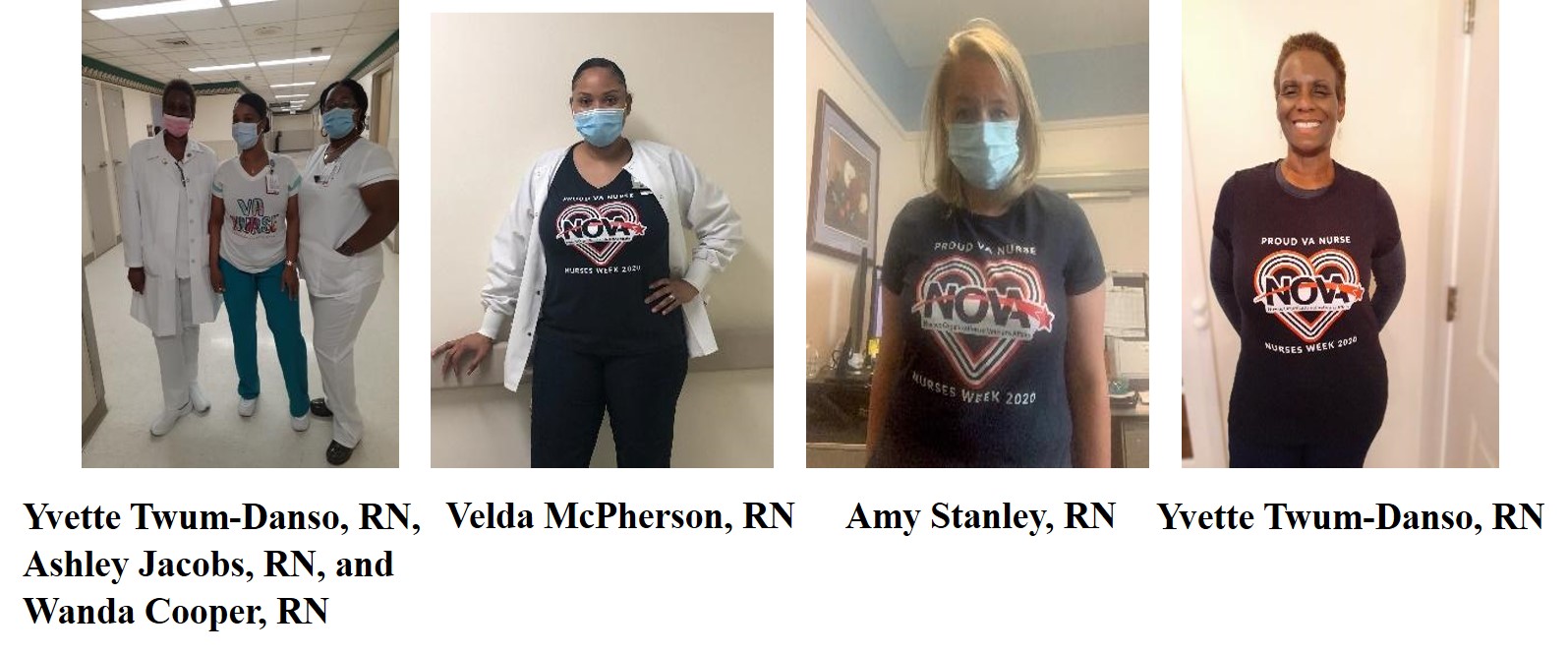

Chapter 362 Achieved Outstanding Nursing Performance
Chapter 362 Welcomes New Members
Eva Rigney recruited by Karen Scott
Dr. Jennifer Stratman recruited by Heather Roth
Sarah Murphy recruited by Yvette Twum-Danso
Harriet Milligan recruited by Maggie Keller
We are grateful beyond measure for good health and phenomenal colleagues during this COVID19 pandemic to encourage, uplift, and inspire!
Please continue to stay strong, resilient, and compassionate!
#ProudVANurses2020!
This post has not been tagged.
Permalink
| Comments (0)
|
  
|
Posted By Ashley Lovelace,
Monday, June 15, 2020
|

Valentina Ward, BSN, RN, MPS, CPPS
NOVA Chapter 226
VA Boston Healthcare System
Boston, MA
Surgery involves counting multiple items, including sponges, needles, blades, instruments, and equipment. This is done as part of the baseline count and in subsequent counts that occur throughout the surgery. On average, it is performed 16 times per surgery, and each of these counts represents an opportunity for error. The perioperative care process during manual counting of surgical items is inherently an error-prone process, and should be supported by the latest evidence-based practice tools to safe-proof the process.
In 2019, the Jamaica Plain (JP) Quality and Safety Forum reviewed the Standardized Operating Procedure (SOP) on “Prevention of Retained Surgical Items (RSIs)”. In order to succeed in revising this fundamental SOP for surgical patient outcomes, I completed the Association of Perioperative Registered Nurses’ Periop Mastery Course on Prevention of RSIs. The first revision was focused on ensuring that the accountability methodology used for all surgical counts to prevent RSIs were standardized and consistent. The second revision of this SOP was done due to the need to incorporate the updates: “Prevention of Retained Surgical Items” of July 2019, the VHA Directive 1103, the AHRQ's recommendations for prevention of foreign body left in during procedure - Patient Safety Indicator 5, The Joint Commission recommendations for healthcare facilities for developing effective processes and procedures for preventing unintended retained foreign objects, the AORN Recommended Practices for Prevention of Retained Surgical Items of 2019, and the VA Boston RCA Action Plan of 2018.
The major update in the last revision is the establishment of the standardized multidisciplinary team-based procedures for counting (both, manually and with RF adjunct technology), documentation of counts, and reconciling count discrepancies for all items used on the surgical field with a goal to zero the risk of patient injury from a retained surgical item. This approach for RSI prevention is multidisciplinary because systems that involve counting and detection are team-based activities that comprise input from multiple perioperative team members. This approach constitutes a primary and proactive strategy to prevent patient harm.
The last revision of the SOP “Prevention of RSIs” incorporated two updated safety tools: The Compendium “OR Team Responsibilities While Resolving Count Discrepancy” and the “Radio Frequency (RF) Scanning Outcome Algorithm”. It was also accompanied by the power-point presentation “Prevention of Retained Surgical Items”, and by the annual Competency Verification Tool for JP OR Perioperative Practices on Prevention of Retained Surgical Items for Circulator RN and Scrub Technician. This is the first SOP to introduce quality and safety metrics for continuous monitoring of the surgical count process and performance improvement.
The Standard Operating Procedure Prevention of Retained Surgical Items was reviewed and approved by the VA Boston Nursing Evidence-Based Practice Committee and became effective in March 2020. An electronic link was set up for distribution to all Veterans Integrated Service Network (VISN) 1 facilities.
As a dedicated nurse at the VA Boston Healthcare System and a NOVA Chapter 226 member, I embrace perioperative care nursing collaboration at the VISN1 level, and I am open to sharing this high-quality standardized procedure with all perioperative NOVA nurses interested in promoting a multidisciplinary team approach to prevention of retained surgical items.
v.peacerain@yahoo.com.
This post has not been tagged.
Permalink
| Comments (0)
|
  
|
Posted By Ashley Lovelace,
Friday, May 29, 2020
|
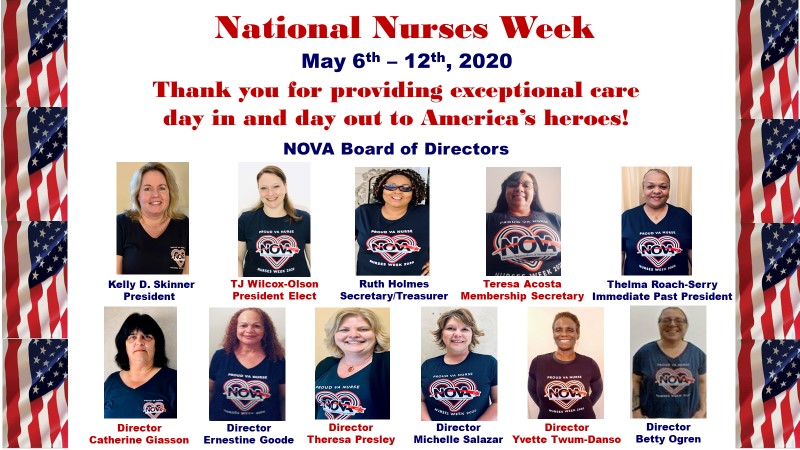
Dear NOVA Members,
On behalf of the National NOVA Board of Directors, I would like to wish you a Happy National Nurses Week. Thank you for providing exceptional care day in and day out to America's heroes amid the global pandemic. Please enjoy this Nurses Week Video which was created as a tribute to every one of you.
Teresa Morris, Director of Advocacy & Government Relations, and I wrote an article entitled: “Veterans Affairs Nurses: Stories from the Front Lines of a Pandemic” that appeared in Veterans Affairs & Military Medicine OUTLOOK and DefenseMediaNetwork.com during Nurses Week. We seized the opportunity to honor VA nurses. Read this article to learn more about VA nurses who deserve special recognition for their nursing excellence, bravery, and compassion during these unprecedented times. The article is featured on pages 22-23 and a NOVA advertisement is displayed on page 72.
2020 is “Year of the Nurse”, therefore, I would like to acknowledge the ongoing fortitude and unyielding commitment of our NOVA members. More than ever, you should be celebrated for your good work and sacrifices, feel appreciated, and have your spirits lifted whenever possible. You continue to risk your personal safety in order to provide exceptional care to our Veterans. You are heroes on the front lines of the coronavirus crisis. It is truly inspiring; makes me proud to be a nurse. Here’s to NOVA nurses, the Best of the Best!
With appreciation,
Kelly D. Skinner
This post has not been tagged.
Permalink
| Comments (0)
|
  
|
Posted By Ashley Lovelace,
Friday, May 29, 2020
|
Shana (Shakhnoza) Rodriguez, BSN, RN, CNOR
NOVA Chapter 420
Central Virginia VA Healthcare System
Richmond, Virginia
VA Nurses are on the frontlines working at the Screening Stations and Drive Through Clinics to rule out and identify Covid-19 positive patients. Those patients are then cared for and treated on the Covid-19 designated inpatient units. Healthcare providers are required to use personal protective equipment (PPE) to protect themselves and others.
Unfortunately, high demand for PPE due to growing numbers of Veterans affected by COVID-19 is depleting available resources for the surgical facial masks. Health care providers and other staff members that are not in direct contact with patients are allowed to wear masks made of cloth.
NOVA Chapter 420 members: Tawanna Smith, Victoria Lewis, Amanda Wall and Linda Droste work on the Spinal Cord Injury & Disorders Units at the Central Virginia VA Healthcare System. I would like to recognize these multitalented nurses that in addition to providing excellent care for our Veterans selflessly stepped up and are offering free cloth masks that they make at home on their own time. They have been busy making cloth masks for people who need them. I believe that this is a valuable gift for anyone these days!
We have all heard that nurses wear many different hats and now masks. I would like to thank Tawanna, Victoria, Amanda and Linda. Their generosity, kindness and everything they do for others is very much appreciated.

Tawanna Smith, Victoria Lewis and Amanda Langford
This post has not been tagged.
Permalink
| Comments (0)
|
  
|
Posted By Ashley Lovelace,
Tuesday, May 26, 2020
|

Vanessa Coronel, BSN, RN
VA Boston Healthcare System
Boston, MA

NOVA Emeritus Member Denise Dulude was one of the first nurses to come out of retirement and olunteer to fight the COVID-19 pandemic. This article will highlight her nursing background at the VA and why she heeded the call to fight this pandemic.
Background
Denise began her VA nursing career in the 1980s. She started as a staff nurse on a neurology floor and later became the Nurse Manager for neurology’s stroke center. Her progression in the clinical and leadership ladder has been impressive- being the nurse manager for several units including Emergency Department, Cardiac Care Unit and Outpatient Specialty Clinics. In her 37-year career in nursing, Denise has been known to be a great mentor to staff, nurse managers and associate chief nurses.
Reasons for Choosing VA
Back in the 1980s, the VA offered to excuse all federal student loans for nurses who worked for two years. As a new nurse faced with student loan payments, Denise considered this a good deal. After two years, she had grown to really appreciate serving the Veterans. Denise shared that “The Veterans truly appreciate you- they have this authenticity that is very hard to describe. The VA is more than just a hospital for our Veterans- it is a meeting place or more like a second home for them. They look forward to interacting with fellow Veterans and they feel true appreciation as reflected by the quality of care that the VA provides. It is only the VA that truly knows our Veterans and how to provide the specialized care that they deserve.”
Nursing Platform of Increasing Vaccinations
In early 2000, Denise was the Patient Care Coordinator in the acute care setting. Being on the night tour, she noticed that nurses did not have access for vaccination and other employee health resources. Typically, employee health was only open during weekdays. Denise began to vaccinate nurses during her leadership rounds. She worked closely with Infection Prevention and after three years, had recruited more nurses to join her in vaccinating the frontline staff. Denise added additional services such as tuberculosis testing and personal protective equipment fitting. In 2010, she spearheaded process improvement projects to increase flu vaccination among Veterans. Hence, Denise is well known at the VA Boston as the original flu fighter.

Denise Dulude administering flu shot to the VA Secretary Robert McDonald in October 2014.

As a Halloween treat. Denise Dulude and Sue Shannon are offering flu shots to employees and Veterans via the rolling flu cart in 2015.
Impact of COVID-19 Pandemic in Nursing
In her 37-year career, Denise has been involved with several disaster response initiatives (Post-9/11, Measles Outbreak, TB Exposure, and Boston Marathon Bombing), however Denise has not seen anything like the COVID-19 pandemic. Although, she can totally relate to the pandemic’s impact in nursing. The majority of the frontline staff dealing with this pandemic are nurses and are putting their own safety at risk and they worry for their own families as well. They are juggling their commitment to providing care and other priorities which is a huge burden and can create a lot of stress.
VA Boston’s Response to the COVID-19 Pandemic
VA Boston has a robust process in ensuring that frontline staff have the appropriate personal protective equipment (PPE). As part of the COVID 19 Incident Management Team’s Personal Protective Equipment Staff, Denise has been spearheading efforts to ensure that frontline staff have the knowledge, competencies and resources to utilize proper PPE appropriately. Her duties include working with the PPE Support Staff to facilitate the proper use of PPE, track inventory and usage levels and visual inspection of VA staff for proper PPE (as shown in the picture below). VA Boston continues to work with other VAs and the private sector to ensure the appropriate PPE par levels. Mitigation strategies are also in place in anticipation of the COVID-19 surge.

Denise Dulude in PPE rounds with Nicole Condon checking if frontline staff have the appropriate PPE.
Lessons Learned from a Pandemic
Denise had three words to say: “Communicate, communicate, communicate. Nurse Leaders need to ensure transparency of information.” Denise mentioned that the VA Boston conducts weekly town hall meetings where executive leadership has an open forum with all employees. Employee Assistance Program (EAP), a confidential program helps VA employees work through various life challenges that may adversely affect their job performance, health or personal well-being. Located on all three campuses, EAP is a helpful resource for employees who find themselves overwhelmed by the pandemic. The Holistic Committee offers meditation and relaxation classes. Most importantly, the VA nursing culture of teamwork persists. As Denise has mentioned: “We are all in it together and we shall overcome this.”
Reason for Coming Out of Retirement to Help Fight Covid-19
Denise mentioned that she goes where help is needed. Perhaps it is inherent in nursing to help others. Denise may have retired but one could ever take the nurse out of Denise. Thank you, Denise, for your dedication to our Veterans and Happy Nurses Week!
This post has not been tagged.
Permalink
| Comments (0)
|
  
|
Posted By Ashley Lovelace,
Tuesday, May 26, 2020
|
Teresa Acosta, DNP, MSN, RN
NOVA Chapter 386
El Paso VA Health Care System, El Paso, TX
NOVA Chapter 386 is currently working on a community service project (non-perishable food drive) benefiting the Veterans Non-Profit Food Pantry (VNP). The VNP is an organization that serves low income Veterans, unemployed Veterans and their immediate family in meeting their most basic needs. During this COVID- 19 crisis, the VNP is facing hardships. They are seeing an increase in Veterans they serve (60 Veteran households being newly registered) running low on food and having to purchase food at market value compared to their usual food purchase of .15 cents per pound. They are in dire need of hamburger helper, peanut butter, canned meals, crackers, cookies, cereal, and canned meat. The VNP has a donate now option on their website at https://www.veteransnonprofit.org/ for anyone that wishes to donate money.
NOVA Chapter 386 received approval from El Paso VA leadership to place donation boxes at VA locations and opened-up the project to all VA employees that wish to participate. William Beaumont Army Medical Center (DoD) nursing was invited to partner in this project with the El Paso VA. In joint efforts, we can serve our Veteran community. We are looking at collecting three weeks in the Month of May. A drive by parade with all the food collected is planned for the last weekend in May to the VNP location.


This post has not been tagged.
Permalink
| Comments (0)
|
  
|
Posted By Ashley Lovelace,
Tuesday, May 26, 2020
|
Shana (Shakhnoza) Rodriguez. BSN, RN, CNOR
NOVA Chapter 420
Central Virginia Healthcare System
Richmond, VA
When someone mentions OR nurses, the first thing that comes to mind is people covered from head to toe with faces hidden behind masks. A lot of people have no idea of what we do behind the red line that divides restricted and non-restricted areas. Even nurses of different specialties have vague ideas of what OR nursing entails, and I often get questions about what exactly our role in the OR is. We can easily get lost in our own hospital because we rarely get out of the OR is an anecdotal truth.
However, while the COVID-19 pandemic is ravaging through our nation, a lot of units need medically trained professionals to provide adequate care for patients arriving at hospitals at an increasing rate. As an answer to the call for help, OR nurses are stepping out to help and support nurses working on the front lines. For example, at the Central Virginia Health Care System in Richmond, Virginia, a lot of our OR nurses were detailed to screen Veterans for COVID-19 at the stations in our Drive-Through Clinic (DTC). Patients arriving with COVID-19 symptoms are tested before they go to the isolation room in the emergency room (ER) to receive medical attention. DTC reduces exposure of the ER employees and other patients with non-COVID-19 emergencies.
 
Picture on left: OR nurses Dena Traylor (Neuro Service) and Adena Mahini (Ortho Service) are screening Veterans at the DTC.
Picture on right: Pamela Liddle (ENT Service Coordinator) trying to warm up during a cold, rainy day while waiting on Veterans arriving at the DTC.
 
Picture on Left: Kristina Kniceley (Vascular Service) and Dena Traylor (Neuro Service) were photographed before screening Veterans for COVID-19 started.
Picture on Right: Tara Stevens (ENT Service) taking care of Veterans at the DTC.
Due to cancellations of elective cases, our newly opened Post-Anesthesia Care Unit 3-E was transformed into a unit specifically for COVID-19 positive patients. ICU nurses floating there are cross training PACU nurses while OR nurses are helping them to don/doff personal protective equipment (PPE) in proper manner preventing contamination. OR nurses are well versed when it comes to infection control and contamination prevention. PACU and ICU nurses verbalized how happy they are and feel protected because the OR RNs are observing and assisting them to put on PPE. Besides observing and teaching other healthcare providers who are consulting on or assessing COVID positive patients, our OR nurses are providing support by running blood gases, bringing extra supplies, medications, etc. to nurses working inside the COVID rooms, so they don’t have to constantly don/doff PPE if they need additional supplies.

Lauren Walden (GU Service) is working on 3-E, COVID-19 Unit.

OR nurses (from left to right): Lauren Walden (GU Service), Courtney Troy (Neuro Service), and Kathleen Childress (GU Service Coordinator) are working with ICU and PACU nurses on the COVID-19 Unit.

Top left to right and bottom left to right: Darla McKimmie (recently joined our VA family and Ophthalmology Service, Kristina Kniceley (Vascular Service), Laura Baxter (Ortho Service), Terrice Wisbang (Cardiac Service), Melinda Talley (General Service), Tamara Kelejian (Neurosurgery Service Coordinator), and Courtney Troy (Neurosurgery Service) are working as observers and instructors for proper donning/doffing of PPE on those units, as well as “runners” for supplies and doing blood gases at the MICU and 3-E, COVID-19 Unit.
Another group of nurses are working at the nursing home and hospice care units. They are helping to provide care for the Veterans residing there or working by the entrances of those units checking healthcare providers’ temperatures before they enter. Since our in-house barber shop is closed due to strict quarantine rules, a lot of Veterans residing in the above mentioned units needed haircuts and shaving. Our Podiatry Service Coordinator, Barrett Smith, bought all the necessary supplies and gave haircuts and shaved the patients on the nursing home and hospice units.
  
Picture on left: Barrett “Barry” Smith is transporting a patient from the nursing home to the Radiology Department for a scheduled test.
Picture in middle and on right:Jeremy Andrion (Ortho Service Coordinator) and Bernadith Abuan (Cardiac Service Coordinator) are working by the entrances to the Nursing Home and Hospice Care Units where they are screening healthcare providers arriving to those units.
At times like this where all hands-on deck is required to serve our Veterans and provide the best possible care to achieve positive outcomes and protect them from Covid-19, our OR nurses did not hesitate to volunteer to be where they are needed. These amazing nurses changed their regular work schedules and are working weekends, evenings, nights, and longer hours to accommodate the needs of the Veterans.
As a wife of a Veteran myself, I simply would like to recognize their selfless service and show my appreciation for their work ethic and dedication for our patients that served our country!
This post has not been tagged.
Permalink
| Comments (0)
|
  
|
Posted By Ashley Lovelace,
Tuesday, May 26, 2020
|
NOVA Chapter 226
Boston, MA
Kelly D. Skinner, DNP, APRN, NP-C, GNP-BC, CRRN, WCC, CFCN
Year of the Nurse
The World Health Organization (WHO) designated 2020 as the “International Year of the Nurse and the Midwife” to recognize the 200th anniversary of Florence Nightingale’s birth. This extends the opportunity to honor nurses beyond the typical Nurses Week celebrations. This year, the NOVA Chapter 226 Board Members wanted to do something special, so we purchased NOVA Nurses Week 2020 t-shirts and created a card to thank our members for all they do for our Veterans.

2020 Nurses Week

Due to the COVID-19 pandemic, our Nurses Week activities this year were done while maintaining social distancing. We kicked off Nurses Week on May 6th with a Military Flyover, a Rolling Rally and a Skype call entitled Happy Nurses Week with Ceci McVey, the Associate Director, Nursing and Patient Care Services. Ceci and our Medical Center Director, Vincent Ng, provided introductory comments and then the 2020 Secretary’s Award for Excellence in Nursing award recipients were recognized. Congratulations to Adrianna Nava, RN (Expanded Role), Diana Santana (RN Role), Gretchen Pomerleau (LPN Role) and Stephanie Henion (HT Role)! The Holistic Committee offered several mindfulness activities such as distance reiki, tapping/Metta meditation, distance yoga, and visualization/energy exercises throughout the week. Tuition vouchers were given away, sessions were available for nurses to receive help with proficiencies and reconsiderations requests, and Nurses Night at Fenway and Healthy Leg Day calls took place. Nurses also sent numerous Thank a Nurse Cards to their colleagues. They even represented their college by wearing college gear and submitting the pictures. We just couldn’t let National Nurse Week go by without honoring our nurses, so we took advantage of the opportunity to celebrate with them virtually!


Happy International Nurses Day!
NOVA member, Genevieve Lemay, who works in the MICU at the VA Boston Healthcare System wishes you a Happy International Nurses Day! In the group photo below, Genevieve (2nd from the left) is with her classmates during their Oath Taking after they passed the Philippine Nursing Boards. There were 100 in her class. This photo is also in honor of their dear classmate (1st from the left) who they recently lost due to cancer.

Class of 1982 Nursing Graduates
Cebu Velez General Hospital Velez College
Welcome Back
The VA received approval and started rehiring retired health care professionals in order to increase staffing during the COVID-19 pandemic. Eileen Pflanz, NOVA Emeritus Member and NOVA Chapter 226 Immediate Past President, who retired in December 2019 and Denise Dulude, NOVA Emeritus Member and Longtime NOVA Member, who retired in January 2020 answered the call to return to duty. NOVA Chapter 226 welcomes them back to the VA Boston Healthcare System and applauds them for their continued service to the Veterans through the coronavirus crisis.
 
Eileen Pflanz Denise Dulude
This post has not been tagged.
Permalink
| Comments (0)
|
  
|
Posted By Ashley Lovelace,
Tuesday, May 26, 2020
|

Penny Kaye Jensen, DNP, APRN, FNP-C, FAAN, FAANP
VACO/ONS
National APRN Program Manager

Ronald Nardi, MSN, APRN, PMHCNS-BC
Alaska VA Healthcare System
Substance Use Disorder, Domiciliary Care, Same Day Access Mental Health APRN
Great news! Penny Kaye Jensen, DNP, FNP-BC, FAAN, FAANP and Mr. Ronald Nardi MSN, APRN, PMHCNS-BC have agreed to serve as chairpersons of the newly formed NOVA Advanced Practice Registered Nurse (APRN) Committee.
Penny Kaye Jensen
Dr. Jensen began her career with the Department of Veterans Affairs in 1994 and has practiced for the past 22 years as a nurse practitioner in the Outpatient Primary Care Clinics at the Salt Lake City Veterans Affairs Healthcare System. She is a Fellow of the American Academy of Nursing (AAN), American Academy of Nurse Practitioners (AANP) and a Distinguished Practitioner and Fellow of the National Academies of Practice (NAP). Dr. Jensen served as President of the American Academy of Nurse Practitioners. She received the Towers Health Policy Pinnacle Award as well as the Loretta C. Ford Award in 2017 for her tireless work to further the NP profession at the national level. She is the only NP in the nation to receive both awards.
Dr. Jensen serves as the National APRN Health Policy Liaison for the Department of Veterans Affairs Office of Nursing Services in Washington, D.C. Her primary responsibility has been to lead the Veterans Health Administration’s (VHA) initiative to approve Full Practice Authority (FPA) for all Advanced Practice Registered Nurses (APRNs) throughout the enterprise. She led the VA FPA initiative which resulted in APRN Final Rule (AP44) being approved, granting full practice authority to APRN roles practicing within the VA: Certified Nurse Practitioner (CNP), Certified Clinical Nurse Specialist (CCNS), and Certified Nurse Midwife (CNM). Dr. Jensen shared that, “it has taken over 10 years for this much anticipated day to arrive, ironically falling on Florence Nightingale’s 200th Birthday! I can proudly report that all 140 VA Healthcare Systems (100%) have amended their bylaws to allow FPA for three of the four roles of APRN practice! Congratulations to Puerto Rico for moving forward!”
Ronald Nardi
Mr. Ronald Nardi graduated from Vanderbilt University School of Nursing where he earned his Master of Science degree in Adult Psychiatric Mental Health Nursing and began his VA career at the Nashville, Tennessee Veterans Administration. It is here where he was afforded the opportunity to serve our Nations’ Heroes and recognize the gift of freedom that was paid by those in the armed forces. As a Clinical Nurse Specialist (CNS), he secured his Advanced Practice Registered Nurse licensure in 1994 and was the first APRN at the Institute of Living in Connecticut to prescribe psychotropic medications on an inpatient basis. Mr. Nardi’s career has spanned a variety of psychiatric settings and roles across the full continuum of care. He has served as staff nurse, research, director of inpatient and intensive outpatient care, PTSD Team, Behavioral Health Interdisciplinary Program (BHIP) Team, Substance Use Disorder including Suboxone Treatment, Primary Care Mental Health Integration (PCMHI), Same Day Access, Domiciliary Care, Teacher and Mentor. As of October 2020, Mr. Nardi will reach a milestone of having served 20 years as an APRN in the VA.
Mr. Nardi is currently working at the Alaska VA, having relocated in 2018. He has joined the Nurse Professional Standards Board and has served in a variety of clinical and leadership roles including Interim Clinical Director for the Alaska VA Mental Health Care Line. APRN Nardi is an inaugural member of the Office of Nursing Services Advanced Practice Registered Nurse Council, Clinical Nurse Specialist Council and APRN Qualification Standards Board.
Mr. Nardi joined NOVA many years ago and presented at his first annual conference in New Orleans on Posttraumatic Stress Disorder. He then went on to join the NOVA Board or Directors as a National Director and then Executive Director as Membership Secretary. Mr. Nardi has served as Chairperson of NOVA’s Annual Meeting for several years. At the 2018 Annual Conference Nursing Strong: Evidence Based Care for America’s Heroes in Richmond, Virginia, he again presented. This time as speaker, he shared his experience as it related to Disaster Emergency Medical Personnel System (DEMPS) and his deployment to Puerto Rico following Hurricane Maria. Nurse Nardi is passionate about Nursing and strengthening and growing NOVA. Mr. Nardi feels that, “It is all about the nurses, all nurses, and what NOVA can do for them. Nurses need to be recognized in bold ways.”
If you are an Advanced Practice Registered Nurse (APRN), please contact NOVA nova@vanurse.org. Several members are APRNs but joined NOVA prior to becoming an APRN. NOVA wants to make sure you are in the appropriate membership category. And, if you are interested in joining the NOVA APRN Committee, please let NOVA know. Email notifications with details for future NOVA APRN Committee Meetings and VA APRN National Town Hall Meetings will be going out soon. Stand by!
  
Pictured (Right to Left): APRN Council, Penny Kaye Jensen and Ronald Nardi, VA APRNs in Puerto Rico
This post has not been tagged.
Permalink
| Comments (0)
|
|
